L’importance du sommeil chez les étudiants
Un article intéressant paru dans LaPresse+ le 17 mars 2017 discutant l’importance du sommeil tant chez les enfants au primaire que ceux au secondaire.
Un article intéressant paru dans LaPresse+ le 17 mars 2017 discutant l’importance du sommeil tant chez les enfants au primaire que ceux au secondaire.
The running meter is a distraction that interferes with medical appointments.”
Dr. Rajendra Kale, former editor CMAJ
Our Facebook post last week on plans to reduce parking fees at Quebec hospitals was our most popular yet. Parking fees can be excessive and their appropriateness has been extensively debated.
In the March 6, 2012 issue of the Canadian Medical Journal (CMAJ), doctors debated the merit and necessity of charging patients for parking. Dr. Tom Closson, President and CEO of the Ontario Hospital Association, argued that parking fees are one of the most common ways of making up the deficit of hospital operating budgets. He stresses that provincial government cutbacks to hospitals eliminate “crucial revenues that hospitals use to fund clinical research and front-line patient care.” He admonishes the Journal’s editorial board, “surely CMAJ has something to say about these and other more relevant issues, instead of banging away on the populist drum about parking fees.
Dr. Tim Meagher of the MUHC takes the opposing position, “I support free hospital parking for patients. I would probably also support free transport to and from hospital visits, reimbursement for time lost from work due to hospital visits, and reimbursement for myriad of ancillary costs that hospital visits generate.”
Dr. Rajendra Kale, editor in chief of the CMAJ, writes “”Parking fees amount to a user fee in disguise.” He urges Canadian hospitals to follow the example set in Scotland and Wales where hospital parking fees are abolished “because they burden (the) patient.” Dr. Kale concludes, “Those opposed to scrapping parking fees for patients need to recognize that such fees are, for all practical purposes, user fees and a barrier to health care. Using revenue generated from such surrogate user fees for health care is against the health policy objective of the Canada Health Act and could become the subject of a legal challenge.”
This opinion was supported by Dr. Brian Goldman, Host of CBC’s White Coat, Black Art, “I think hospital parking fees should be abolished because they punish patients.”
The highlights of the new hospital parking plan, starting April 1, are:
• Hospital visitors will be able to park for free at hospitals in Quebec for the first 30 minutes, instead of paying as much as $10 for that first half hour.
• A flat daily rate will not be applied until a vehicle has been parked for more than four hours, a big change from the current practice of charging the maximum daily rate after 90 minutes.
• Health care institutions must offer weekly and monthly parking passes, as well as books of tickets, at reduced rates.
• Health care institutions must offer daily parking passes that allow motorists to come and go without penalty.

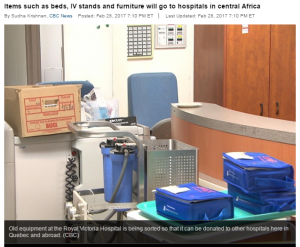
A nice story in the Gazette this week about sharing used medical equipment in Third World countries.
Furniture, bedside tables, equipment from the old Royal Victoria Hospital will be sent to Central Africa to be used in eight hospitals in Cameroon.
Numerous organizations are identified by the World Health Organization to help distribute medical supplies, equipment, vaccines and donations:
HTTP://WWW.WHO.INT/MEDICAL_DEVICES/MANAGEMENT_USE/DONATION_ORG_ROLES.PDF





In Canada, HOPE and HPIC are two organizations that help with this cause.
HPIC (Health Partners International of Canada) is a relief and development organization dedicated to increasing access to medicine and improving health in the developing world.
HPIC is an independent charity that receives donations of medicines, vaccines and medical supplies from Canadian pharmaceutical and healthcare products companies, to be used for humanitarian purposes. HPIC is funded in part by the Government of Canada, foundations, companies and individuals.

Since 2012, Santé Kildare has sent supplies to JustWorld International to support the medical clinic located in Jocotenango, Guatemala. Promoted through the international equestrian community, JustWorld supports basic education, nutrition, health & hygiene, and cultural development programs for children in impoverished communities in Cambodia, Guatemala, and Honduras.
Regrettably, medical equipment donated to developing nations is not always used.
While medical equipment donations in theory enable hospitals in developing countries to receive expensive and advanced technology, in reality much of the equipment breaks easily and is not repaired.
A study of seven hospitals in Haiti found that only 1/3 of the 115 pieces of medical equipment donated after the 2010 earthquake was working after 3 years and 1/2 of the broken equipment could not be repaired. Some of the donated devices, such as incubators for premature babies, were never used because of insufficient electrical voltage in Haiti.
The World Health Organization (WHO) estimates that only 10-30% of all medical equipment donations are ever put into operation. Not only does the equipment need to be donated, it needs to be shipped, delivered, installed, and the local staff trained.
To address this concern, WHO defined 4 principles for a good medical equipment donation:

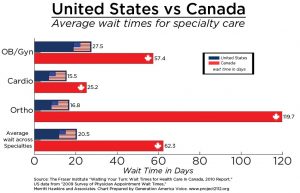
It is no secret that we are (extremely) frustrated with long waiting times. Consecutive governments repeatedly promise to fix this problem but wait times only seem to grow longer.
As noted by the Fraser Institute: “excessively long wait times remain a defining characteristic of Canada’s health-care system, but this year (2016) is the longest we’ve ever seen and that should trouble all Canadians.” Bacchus Barua, senior economist at the Institute, continues, “long wait times aren’t simply minor inconveniences, they can result in increased suffering for patients, lost productivity at work, a decreased quality of life, and in the worst cases, disability or death.”
http://globalnews.ca/news/3083826/medical-wait-times-in-canada-are-longer-than-ever-hitting-20-weeks-in-2016-fraser-institute/
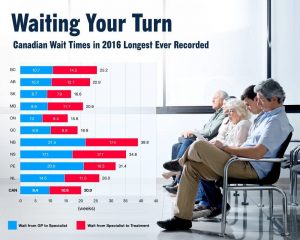
The Canadian Institute of Health Information (CIHI) released a report based on The Commonwealth Fund’s 2016 international survey that highlighted this continued issue. According to the survey, Canada scored the poorest of all 11 countries surveyed when it came to access to specialists. Fifty-six percent of Canadians wait longer than a month to see a specialist—as compared to the international average of 36 percent.
Dr. Josh Tepper, CEO of Health Quality Ontario, along with Vanessa Milne and Sachin Pendharkar, published “Four ways Canada can shorten wait times for specialists” at Healthydebate.ca. Their prescription for success focuses on simple, achievable concepts:
1.Do virtual consults, not visits
Not every patient needs to see a specialist. Often the family physician needs some guidance and a virtual consult system can help.
The Rapid Access to Consultative Expertise (RACE) is a phone based system available in parts of British Columbia. Family physicians call a central phone number during business hours on weekdays, and a specialist calls back within a couple of hours.
The success of RACE in B.C. inspired a similar program in Ontario, called The Champlain BASE e-Consult service. In this system, primary care providers complete a form that includes patient information and the medical question. Test results and images can be attached. The information is then sent to a specialist.
From 2010 to 2015, the BASE service was used in over 10,000 consultations in the Champlain region. The average wait time for a response from the specialist was two days. Most impressively, in 40% of cases the patient did not need to see the specialist.
2.Add physician directories and e-referrals
Alberta currently offers paperless referrals through e-Referrals. The system includes referrals to Oncologists and Orthopedics. Family doctors get an idea of wait times BEFORE submitting the referral and can chose a specific specialist.
3.Try pre-assessment in specialized clinics
Another approach is adding an assessment step in between the referral and the specialist. This method has been successfully introduced for patients with severe low back pain (Interprofessional Spine Assessment and Education Clinics (ISAEC)).
Known as CareAxis in B.C., Saskatchewan, Ontario and Quebec, wait times are reduced by training physiotherapists to triage potential surgical candidates.
4.Switch to central intake
Pooled referral systems (aka central intakes) allow family doctors to select a specific specialist or the first-available. Newfoundland, Ontario, Saskatchewan and Calgary all use this model. Quebec’s model, CRDS, launched in the Fall of 2016, offers central intake for 9 specialties: Cardiology, ENT, Gastroenterology, General Pediatrics, Nephrology, Neurology, Ophthalmology, Orthopedics, and Urology.
Information can be found at:
Tél. : 514-762-CRDS (2737)
Téléc.: 514-732-5121
Courriel: crdsmontreal.ccsmtl@ssss.gouv.qc.ca
So…can wait times be fixed?
All four models can help reduce wait times and simplify the process. However, the authors caution, “Canada is notorious for being a land of pilot projects in health care, where good ideas aren’t scaled well. For systems like this, where getting buy-in from many professionals is crucial, that problem is especially important to overcome.”
Thank you Dr. Brian Goldman for supporting my profession. I went to Mcgill University and studied dietetics and human nutrition which included 4 levels of stage. It takes 3 and half years to complete this program and when you graduate you become an expert in the field of nutrition care. I will admit that I did not feel like an expert until I had accumulated a certain amount of professional experience. Currently, I work at GMF Kildare. If you want to know what a GMF is click here. I also work at CLSC Benny Farm.
Dietitians help patients with such a wide variety of issues. I help the bulk of my patients with chronic disease state management for such illnesses as diabetes, high blood pressure, sub-optimal cholesterol and of course weight management. Sometimes I see seniors that appear malnourished. This can be very serious and requires a skilled intervention to prevent further complications. I have colleagues who specialize in pediatric nutrition and prenatal care and others who are experts in tube feeding on surgical units in acute care. Another colleague is a home care specialist and provides direct nutrition care in patients own living environment. Some dietitians are even food service managers who run the acute care, rehab and long term care kitchens; ensuring that patients receive appropriate meals and snacks.
The first time I meet a new patient I will do an initial evaluation. This can take about an hour. I will ask many health related and social questions to fully understand the client’s lifestyle habits. This information will help make me the right assessment and give the appropriate intervention for that client. It’s important to understand that each nutrition care intervention is individualized and created just for that person. This is what I am trained to do and how I am able to help people. It is just like doctors who are trained to ask the right questions, make the proper diagnosis and provide the right treatment for each patient they see.
There are so many variables that make up a person’s medical and social history. Each person’s experience is going to determine what type of nutrition care they will need. It’s very important to get a sense of what the patient is willing to change. As a professional dietitian, I must be able to work with where the patient is at, on any given day. I need to ask, are they ready to make a big change like reducing simple sugars or are they willing to try something a bit easier like add a glass of water to their daily intake? Sometimes it takes many nutrition care follow ups before a client is even willing to think about changing a behavior.
I provide information concerning the management, of a disease or condition, but it is the patient’s responsibility to use the information to promote change. The patient always has the right to make the choice that works for them and sometimes that means not following dietary advice. Not everybody is ready to work on their diet and lifestyle habits. Either way, I provide motivation and can coach clients wherever they may be on the behavioral change continuum.
Caryn Roll
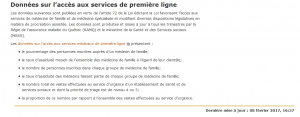
“Created to improve access, Montreal clinics often turn away patients,” published in the Gazette on February 15, 2017, is a misleading and misrepresentative article. It makes false assumptions and reaches incorrect conclusions.
The article states that “there are 86 family medicine groups in Montreal that rely on government funding to stay open longer than private doctors’ offices.” The author contends that “fewer than half the clinics are actually open seven days a week.”
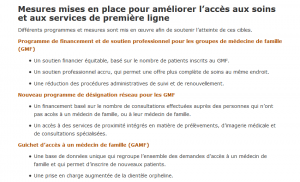
The reality is GMFs are neither super-clinics nor general walk-ins. They are grouped, private, family medicine practices that offer care to a defined, registered patient population. Emphasis is placed on assiduité, fidélisation and prise en charge. In other words, GMFs prioritize their own patients while super-clinics or GMF-reseau (known previously as cliniques-reseau) are designed primarily for patients who do not have a family doctor.
These distinctions are available at: http://www.msss.gouv.qc.ca/professionnels/statistiques-donnees-services-sante-services-sociaux/acces-premiere-ligne/ and http://sante.gouv.qc.ca/systeme-sante-en-bref/groupe-de-medecine-de-famille-gmf/.
GMFs do not all receive the same funding and are not expected to maintain the same number of operating hours or days. While larger GMFs are open 68 hours/week, smaller GMFs only need to be open 5 or 6 days/week.
Yes – GMF walk-in clinics generally extend appointments to non-registered patients whenever possible. “All” patients can come irrespective of age, gender or medical history. Clinics, doctors, nurses are all working to improve access and help patients in need. But the GMF is not a “general” walk-in clinic – and hasn’t been since their inception in the early 2000s.
At the end of the day, the article should have asked – “can patients obtain timely appointments with their own family doctor?” Bottom line – register with a family doctor.



“We are drowning in information but starved for knowledge.” John Naibitt
“We can just Google it!” writes Dr. Jalees Rehman of the University of Illinois at Chicago in Scientific America on August 2, 2012. “Identifying the websites with the most accurate and relevant information are critical skills that are necessary for navigating our way in the digital information jungle, but unfortunately, these skills are rarely taught. In most cases, inaccurate or irrelevant information on the internet merely delays us for a few minutes until we do find the answer to what we are looking for. However, when it comes to medical information, inaccurate or irrelevant information could potentially have a major detrimental impact on our well-being.
I invite you visit the sites below (and at our newest website feature: Patient Resources –www.santekildare.ca/services/patient-resources/) which provide diverse, relevant and reliable medical information. Some help calculate risk for cancer, osteoporosis and heart disease, while others prepare patients for appointments, review medications, discuss controversies in screening and limitations in treatments, and provide patients with easy-to-understand information about prevention and management of common illnesses.
With apologies to J.K.Rowling, “Understanding is the first step to healing.”

CTFPHC
The Canadian Task Force on Preventive Health Care (CTFPHC) has been established by the Public Health Agency of Canada (PHAC) to develop clinical practice guidelines that support primary care providers in delivering preventive health care.
Patient Engagement in Guideline Development: The CTFPHC involves members of the public in its guideline development process. Specifically, the CTFPHC uses feedback from the public to guide the search for evidence on the guideline topic and to develop knowledge translation tools to accompany the guidelines
http://canadiantaskforce.ca/tools-resources/videos/
http://canadiantaskforce.ca/general-public/general-information/
Choosing Wisely Canada
Choosing Wisely Canada is a campaign to help physicians and patients engage in conversations about unnecessary tests, treatments and procedures, and to help physicians and patients make smart and effective choices to ensure high-quality care. Unnecessary tests, treatments and procedures do not add value to care. In fact, they take away from care by potentially exposing patients to harm, leading to more testing to investigate false positives and contributing to stress for patients. And of course unnecessary tests, treatments and procedures put increased strain on the resources of our health care system.

My CancerIQ
Designed by Cancer Care Ontario (CCO), My CancerIQ is a website that helps you understand your risk for cancer and what you can do to help lower that risk.
A series of risk assessments estimate your risk of cancer compared with other Ontarians of the same sex age 40 and over. At the end of each assessment you’ll receive a personalized risk assessment and action plan with tips and resources based on your personal risk factors.
Lung Foundation Australia
Lung Foundation Australia Primary Care Respiratory Toolkit supports the promotion of lung health as well as the early diagnosis and best practice management of lung disease. Evidence shows that Chronic Obstructive Pulmonary Disease is under-recognised, under-diagnosed and under-managed. The Primary Care Respiratory Toolkit has been developed to redress this.
The Lung Age Estimator has been developed to support clinicians to motivate current smokers to quit, by providing a graphic illustration of estimated lung age.
http://doctorwidget.com/alf/ignition/index.php/alf_pcrt#

Medstopper
Medstopper is a tool to help clinicians and patients make decisions about reducing or stopping medications. By entering the list of medications a patient is receiving, Medstopper sequences the drugs from “more likely to stop” to “less likely to stop”, based on three key criteria: the potential of the drug to improve symptoms, its potential to reduce the risk of future illness and its likelihood of causing harm. Suggestions for how to taper the medication are also provided.
Canadian Patient Safety Institute
Established by Health Canada in 2003, the Canadian Patient Safety Institute (CPSI) works with governments, health organizations, leaders, and healthcare providers to inspire extraordinary improvement in patient safety and quality.
Shift to Safety offers tips and tools for talking to you healthcare team. Empower yourself with information to help you ask good questions, connect with the right people, and learn as much as you can to keep you or a family member safe while receiving healthcare.
http://www.patientsafetyinstitute.ca/en/toolsresources/questions-are-the-answer/pages/default.aspx

Calorie Counter
How many calories should you eat? One-size-fits all recommendation do not work – each plan needs to be customized to each individual. Science tells us that 1 pound of fat is equal to 3500 calories so, in theory, a daily calorie deficit of 500 should result in 1 pound per week fat loss. Regrettably, in reality things don’t quite work that efficiently.
http://www.bmimedical.ca/calculator.aspx

CVD Calculator
This Cardiovascular disease (CVD) calculator from the Therapeutics Education Collaboration uses both Framingham and the new ASCVD formulas. It displays benefit estimates for all treatments – diet, lifestyle and medications. The calculator promotes itself as the BEST tool for calculating cardiovascular risk.
http://chd.bestsciencemedicine.com/calc2.html

Journal of the American Medical Association
Explore the latest patient information from The JAMA Network, including easy-to-understand information about prevention and management of common illnesses.
http://jamanetwork.com/collections/6258/for-patients
Calcium Calculator
Fracture Risk Assessment

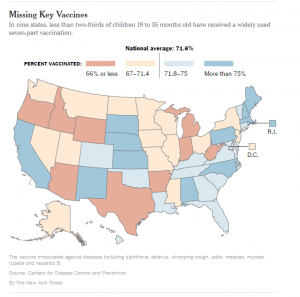
Update on Measles
-No cases reported in Canada in 2017
-11 cases reported in Canada in 2016
-In January 2017, 23 people from 6 states (California, Colorado, Florida, New Jersey, New York, and Pennsylvania) were reported to have measles.
-In 2016, 70 people from 16 states were reported to have measles.
• The majority of people who got measles were unvaccinated.
• Measles is still common in many parts of the world including some countries in Europe, Asia, the Pacific, and Africa.
• Travelers with measles continue to bring the disease into the U.S. and Canada
• Measles can spread when it reaches a community where groups of people are unvaccinated.
What is Measles?
Measles is a highly contagious viral disease. It remains an important cause of death among young children globally, despite the availability of a safe and effective vaccine.
How is it transmitted?
Measles is transmitted via droplets from the nose, mouth or throat of infected persons.
What are the symptoms?
Initial symptoms, which usually appear 10–12 days after infection, include high fever, a runny nose, bloodshot eyes, and tiny white spots on the inside of the mouth. Several days later, a rash develops, starting on the face and upper neck and gradually spreading downwards.
Can it be severe?
The most serious complications include blindness, encephalitis (an infection that causes brain swelling), severe diarrhea and related dehydration, and severe respiratory infections such as pneumonia.
Is it still common?
While global measles deaths have decreased by 75 percent worldwide in recent years — from 544,000 deaths in 2000 to 146,000 in 2013 — measles is still common in many developing countries, particularly in parts of Africa and Asia. More than 20 million people are affected by measles each year. The overwhelming majority (more than 95%) of measles deaths occur in countries with low per capita incomes and weak health infrastructures.
Can measles be prevented?
Yes. The measles vaccine has been in use since the 1960s. It is safe, effective and inexpensive. WHO (World Health Organization) recommends immunization for all susceptible children and adults for whom measles vaccination is not contraindicated.
What is the global plan?
Under the Global Vaccine Action Plan, measles and rubella are targeted for elimination in five WHO Regions by 2020. WHO is the lead technical agency responsible for coordination of immunization and surveillance activities supporting all countries to achieve this goal.
Recent Measles Outbreaks


“The goal of proximity medicine is to keep as many services as possible within people’s reach.”
Dr. Marie-Dominique Beaulieu, former President of the College of Family Physicians of Canada, presented a compelling vision for Family Medicine at the Dr. Ian McWhinney Lecture last September. Entitled “The perils and the promise of proximity,” Dr. Bealieu issues a sincere wake-up call to family doctors, to move “beyond our current understanding of patient-centered care into the realm of partnerships with patients, wherever they are in their lives or communities.”
“Medicine is coming up against a wall.”
Proximity medicine is not simply geographic access – it is a medical approach “that can take into consideration individuals in their entirety and in their complexity, support them in their journey, and place them at the heart of the health care system.” Dr. Beaulieu laments that “technological developments are distancing us from the knowledge, skills, and know-how we need to cope with the challenges facing us.”
The Four Challenges:
1. action on the social determinants of health;
2. timely access to care;
3. care transitions and service integration; and
4. overdiagnosis and overtreatment—our practice of maximally intrusive medicine.
1. Social determinants of health
“We are not all born equal”
Family physicians need to take specific actions aimed at social determinants and by adopting non-stigmatizing practices. This can be accomplished by applying for income supplements, advocating for change in our communities, supporting resources and fostering social participation. Most importantly, ensuring all services are accessible to all our patients, regardless of their sociodemographic characteristics.
2. Accessibility
“We have built fortified castles around our clinics”
Dr. Beaulieu notes that to many, “the concept of service quality referred primarily to whether practices conformed to guidelines rather than to comprehensiveness, timely access, or continuity of care.” To the contrary, timely access to care is not a luxury, but a necessity – or as she writes, “one of the pillars of the patient’s Medical Home.”
3. Care transitions
“The hospital is part of the community and needs to build bridges with services and professionals outside its walls… How do we persuade hospitals to be part of the proximity medicine community?”
“Fragmentation of care is a scourge, one of the primary causes of gaps in care and medical errors.” Care transitions, whether from home to hospital or hospital to home, need to be seamless.
4. Overdiagnosis and overtreatment: “maximally disruptive medicine.”
“Being a patient has become a full-time job”
Dr. Beaulieu laments that over-testing and over-diagnosis have plunged medicine and society into “a vortex from which we cannot extract ourselves without a drastic change in culture.”
“We offer people increasingly complex treatment plans. We interfere with their work, their leisure, and their lives overall. “
The cure: parsimonious medicine not personalized medicine. Evidence-based approaches that propose interventions that offer real differences for patients. “We need a medicine that truly involves patients as full partners in their own diagnoses and care, which is what proximity medicine is all about. We need darn good clinicians.” Medicine based on “sound clinical judgment…medicine that tolerates uncertainty.”
In the end, I agree with Dr. Josh Tepper, CEO and President of Health Quality Ontario:
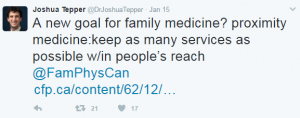
Can Fam Physician. 2016 Dec; 62(12): 964–968.

Santé Kildare was selected to participate in the University of Toronto Department of Family and Community Medicine Quality Improvement “teaming” project in 2016. High functioning primary care teams were chosen across Canada with the goal of developing a blueprint and action plan to guide primary care teams to function effectively. The ultimate outcome leading to improved health of populations, improved and patient and provider experiences and improved value. Santé Kildare was the only clinic studied from Quebec.
Launched in late 2014, the Quality Improvement (QI) Program set out to answer the question: What makes primary care teams effective or high-functioning?
“The evolution of health care provision in the community is moving from a single primary care provider (usually a family physician) providing health care patient by patient in a reactive context, to an organizational one – a primary care team proactively meeting the needs of a defined population. Teaming – a verb – refers to the collective actions or processes associated with a primary health care team performing optimally”.
In April 2016, the environmental scan for the teaming project was completed with case studies of nominated, high-functioning primary care teams. The case studies, representing teams from Alberta, Ontario and Quebec, marked the last element of the scan that included a robust literature review and a series of expert interviews.
Last Fall, the Quality Improvement (QI) Program published themes that were identified as attributes of high-functioning teams. They include:
It was pleasure for Santé Kildare to participate in this project. The full report can be found here.